By Luz E. Ortiz
The neonatal intensive care unit (NICU) is where you will find the smallest and cutest patients.
Newborns may become temporary residents of the NICU if additional medical care is needed for complications such as pre-term birth, congenital conditions, and low-weight birth. A “full-term” baby is born between weeks 38 and 40+ of gestational age. In contrast, babies born at 37 weeks or earlier are considered “pre-term” or “premature,” accounting for about 10% of all live births in the US in 20221. Though the risk of infant mortality increases as births occur earlier in pregnancy, medical advancements have equipped certain NICUs across the nation to care for neonatal patients born as early as 22 weeks!
NICU patients rely on the expertise of their medical team for appropriate and timely diagnoses and treatments. However, assessing symptoms in the NICU can be challenging since the patients can’t communicate verbally! Instead, the medical team must assess the behavioral and physiological changes of each patient, closely monitoring changes in heart rate, blood pressure, limb movement, facial expressions, sleep patterns, temperature, and other parameters.
Additionally, this attentive monitoring must occur around the clock. Each tiny NICU patient is connected to a multitude of cables, monitors, and sensors to collect mountains of real-time data (Figure 1). Medical providers continually interpret these data to ensure the best care, manage pain, and increase survival chances for these adorable patients. Although NICU medical staff provide expert care, the neonatal mortality rate in the US increased by 3% in 20222. This somber statistic highlights the need to improve healthcare protocols and technology to maximize the chances of survival for premature patients.

Artificial intelligence (AI) is becoming a potential tool for monitoring vital signs, predicting diseases, assessing risks, and carrying out diagnostics in neonatal care. If successful, efforts to introduce AI into routine NICU care have the potential to improve these tiny patients’ chances of survival. AI tools are being investigated in several areas of neonatal care, including neuromonitoring, pain analysis, and respiratory assessment.
AI in neonatal neuromonitoring
Pre-term babies are at a higher risk of developing seizures compared to their full-term counterparts mainly due to brain immaturity3,4. Seizures can be detrimental to neurological function, and a fast response is critical for preventing further damage. Identifying seizures in NICU patients can be tricky since most seizures in premature neonatal patients are non-convulsive and can only be identified by direct neuromonitoring5. Neuromonitoring in neonates is achieved with electroencephalograms (EEG), which are non-invasive recordings of the electrical activity in the patient’s cerebral cortex (the brain’s outermost layer). EEG readings are critical for identifying epileptic seizures and differentiating epileptic activity from nonepileptic neurological events.
Analyzing large amounts of continuously gathered EEG data requires the expertise of neurophysiologists, the availability of whom can be a challenge in an understaffed NICU. An AI-based algorithm developed in 2020 by the INFANT Research Centre in Cork, Ireland attempts to mitigate understaffing by analyzing and interpreting EEG data for automatic identification and detection of seizure events6. Additionally, some algorithms can extract information from EEG readings to rank the severity of another serious neonatal condition, perinatal hypoxic-ischemic encephalopathy (HIE)7,8. HIE is a type of brain injury caused by a lack of oxygenated blood flow to regions of the brain immediately before, during, or after birth. AI monitors for HIE could expedite the identification of these events, thereby potentially saving lives by enabling rapid medical intervention.
AI in neonatal pain recognition
Upon arrival at the NICU, neonates undergo medical procedures that cause discomfort and pain. Blood draws from sensitive parts of the body (arms, legs, and fingers), intravenous (IV) needle placement and re-placement (arms, hands, legs, and/or head!), among others, are routine procedures in the NICU. If a patient’s condition is severe upon arrival, these procedures must occur urgently – so quickly that, at times, no pain medication is provided.
Pain assessment is traditionally performed by the medical care team, and this assessment requires constant monitoring. In 2022, researchers at Zhejiang University School of Medicine in Hangzhou, China developed an AI-based neonatal pain assessment algorithm using video recordings of infants’ facial expressions during routine blood draws. Based on a sample size of 232 newborns, the algorithm correctly detected and scored pain 89% of the time compared to human nurses’ assessments of the same pain response behaviors9.
Commonly, NICU patients must undergo surgery, sometimes undergoing multiple procedures in a short period of time, leading to post-operative inflammation and pain. The opioids fentanyl and morphine are the current drugs of choice to manage postsurgical pain in neonates. These drugs are fast-acting, effective, and potent, but also highly addictive. Neonates exposed to these narcotics require a careful tapering process prior to being discharged10. In 2020, a group from the University of South Florida proposed the first fully AI-based system for assessing postoperative pain onset and intensity in neonates11. Accurate and early prediction of postsurgical pain onset would allow caregivers to alleviate pain with slower-acting non-opioid drugs and decrease the risk of opioid withdrawal.
AI in neonatal respiratory assessment
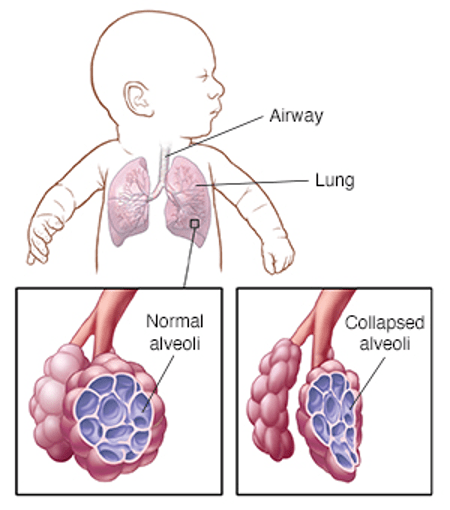
Most babies born before 29 weeks of gestational age are affected by respiratory distress syndrome (RDS), a serious condition that makes it difficult for babies to breathe7. RDS is caused by insufficient levels of surfactant, a lipid-protein substance produced by type II pneumocytes in the alveoli (tiny air sacs) of the lungs. Surfactant is essential for lowering the surface tension in the lungs by allowing the alveoli to remain open for oxygen and carbon dioxide exchange. In the absence of adequate levels of surfactant, the alveoli no longer expand with each breath, preventing proper oxygenation and resulting in lung collapse12 (Figure 2). Currently, lung ultrasounds are used to monitor lung health and assess the risk of RDS and other lung complications. A group from the University of Federico II in Naples, Italy reported that an AI-based analysis of 600 lung ultrasounds from infants with varying degrees of respiratory underdevelopment successfully quantified levels of air circulation and degrees of respiratory distress13.
AI has the potential to radically change neonatal care by assisting in diagnosis, assessment, and medical decision-making. The examples discussed above are only a few areas where AI is being explored to enhance neonatal care. Other groups are researching the utility of AI for procedures like eye examinations, vital signs monitoring, early prediction of intestinal perforation, and jaundice detection and monitoring. Integrating these AI-based systems into NICU routine practices internationally will be the next challenge; however, it looks like some level of implementation in the NICU is plausible. In 2022, the Children’s Hospital Association reported the opening of the Borowy Family Children’s Critical Care Tower at the Wolfson Children’s Hospital in Jacksonville, Florida. This NICU is currently using AI-based monitoring and analysis of vitals, lab results, and magnetic resonance imaging (MRI) with the aim of assisting healthcare providers in predicting health trends. Thanks to AI advancements, the future of neonatal care looks promising!
TL;DR
- Premature or pre-term neonates usually need extensive medical care after birth.
- The neonatal intensive care unit (NICU) collects large amounts of data that can be used for AI-based monitoring and assessment of potential symptoms.
- AI-based algorithms have successfully detected and assessed neonatal pain, seizures, and lung complications.
- Integration of AI-based approaches in the NICU may radically improve survival chances for these tiny patients.
Reference
- Michelle J.K. Osterman MHS, Brady E. Hamilton, Ph.D., Joyce A. Martin, M.P.H., Anne K. Driscoll, Ph.D.,, and Claudia P. Valenzuela MPH. Births: Final Data for 2022. National Vital Statistics System: National Vital Statistics Report; 2024.
- Danielle M. Ely PD, and Anne K. Driscoll, Ph.D. Infant Mortality in the United States: Provisional Data From the 2022 Period Linked Birth/Infant Death File. 2023.
- Spagnoli C, Falsaperla R, Deolmi M, et al. Symptomatic seizures in preterm newborns: a review on clinical features and prognosis. Ital J Pediatr 2018;44(1):115, doi:10.1186/s13052-018-0573-y
- Abbott A. Neuroscience: The brain, interrupted. Nature 2015;518(7537):24-6, doi:10.1038/518024a
- Murray DM, Boylan GB, Ali I, et al. Defining the gap between electrographic seizure burden, clinical expression and staff recognition of neonatal seizures. Arch Dis Child Fetal Neonatal Ed 2008;93(3):F187-91, doi:10.1136/adc.2005.086314
- Pavel AM, Rennie JM, de Vries LS, et al. A machine-learning algorithm for neonatal seizure recognition: a multicentre, randomised, controlled trial. Lancet Child Adolesc Health 2020;4(10):740-749, doi:10.1016/S2352-4642(20)30239-X
- Chioma R, Sbordone A, Patti ML, et al. Applications of Artificial Intelligence in Neonatology. . 2023;13(3211, doi:https://doi.org/10.3390/app13053211
- Pavel AM, O’Toole JM, Proietti J, et al. Machine learning for the early prediction of infants with electrographic seizures in neonatal hypoxic-ischemic encephalopathy. Epilepsia 2023;64(2):456-468, doi:10.1111/epi.17468
- Cheng X, Zhu H, Mei L, et al. Artificial Intelligence Based Pain Assessment Technology in Clinical Application of Real-World Neonatal Blood Sampling. Diagnostics (Basel) 2022;12(8), doi:10.3390/diagnostics12081831
- Salekin MS, Mouton PR, Zamzmi G, et al. Future roles of artificial intelligence in early pain management of newborns. Paediatr Neonatal Pain 2021;3(3):134-145, doi:10.1002/pne2.12060
- M. S. Salekin GZ, D. Goldgof, R. Kasturi, T. Ho and Y. Sun. First Investigation into the Use of Deep Learning for Continuous Assessment of Neonatal Postoperative Pain. 15th IEEE International Conference on Automatic Face and Gesture Recognition (FG2020), Buenos Aires, Argentina, 2020, pp. 415-419.; 2020.
- Han S, Mallampalli RK. The Role of Surfactant in Lung Disease and Host Defense against Pulmonary Infections. Ann Am Thorac Soc 2015;12(5):765-74, doi:10.1513/AnnalsATS.201411-507FR
- Raimondi F, Migliaro F, Verdoliva L, et al. Visual assessment versus computer-assisted gray scale analysis in the ultrasound evaluation of neonatal respiratory status. PLoS One 2018;13(10):e0202397, doi:10.1371/journal.pone.0202397