By Victoria Vernail
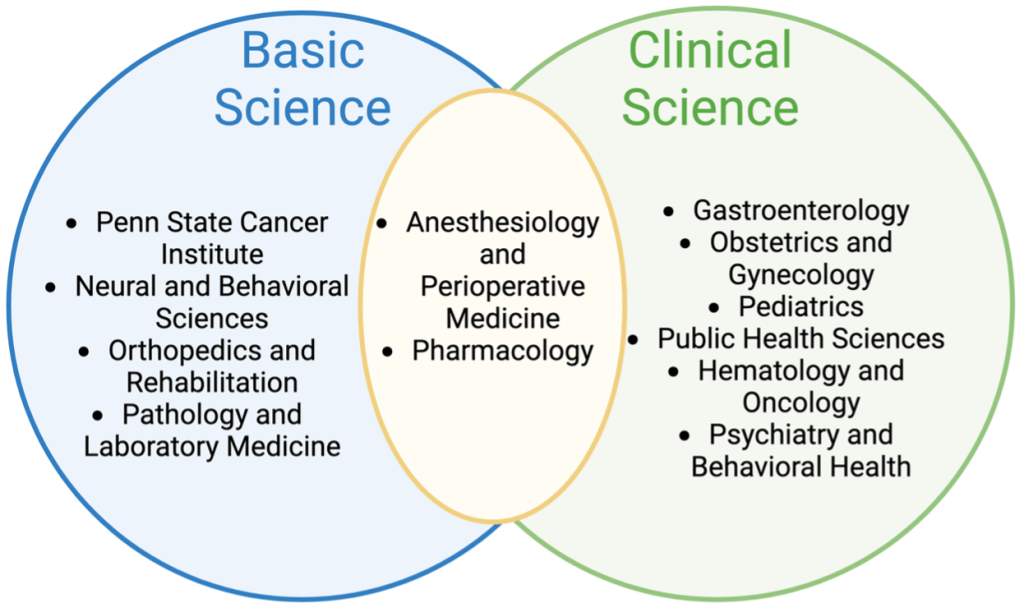
If you give a mouse medical marijuana… Could it treat cancer? Does it minimize pain? Can it decrease anxiety? Does it lower blood pressure? The Penn State College of Medicine (COM) is trying to answer these questions and more through the Medical Marijuana Academic Clinical Research Center (MMACRC). This collaborative research effort spans several basic science disciplines and includes clinicians across departments (Figure 1). The center supports 3 colleges, 12 unique departments, and 20+ research laboratories. I sat down with Dr. Kent Vrana, the director of the Penn State MMACRC, to learn more about the history, achievements, and future goals of the MMACRC.
History
The MMACRC was established in 2019 to expand research into medical marijuana following the drug’s legalization for medical use in Pennsylvania in 2016. The legalization of medical marijuana highlighted the need for an environment where adult patients can get access to safe medicines through medical marijuana dispensaries. In response, Penn State formed a sponsored research agreement between the College of Medicine and PA Options for Wellness to increase research into medical cannabis and facilitate cool, new, collaborative research. If investigators have an idea that is exciting and fits a need, the MMACRC can provide funds to support the research. This model lends itself to a broad scope of research across departments and disciplines. There are two divisions of the MMACRC: the basic science (preclinical) division and the clinical division. Researchers from each division tackle scientific questions from different perspectives and meet to discuss findings. While each division meets regularly on their own, the MMACRC also holds annual retreats where all MMACRC researchers exchange ideas and share recent developments.
Research Significance
In our conversation, Dr. Vrana shared that the greatest accomplishments of the MMACRC to date have been increasing awareness and helping researchers to enter the field. Many MMACRC laboratories have other primary focuses but because medical marijuana use is increasing in a variety of therapeutic settings, there is a greater need to research the benefits and dangers.1 Therefore, research from the MMACRC examines the use of cannabinoids in the context of cancer, inflammatory bowel disease, pain, cardiovascular function, and stress-related disorders. More than 25 papers have been published by the MMACRC in the four years that it has been funded.
The MMACRC enables researchers to conduct research on the chemical components of the cannabis plant, which previously may have been inaccessible due to regulations. The biological compounds of interest, known as cannabinoids, include cannabidiol (CBD), tetrahydrocannabinol (THC), and the parent compound of CBD and THC, cannabigerol (CBG) (Figure 2).2

The increasing use of medical marijuana as a therapeutic tool drives an increased need for preclinical research on cannabinoid mechanism of action. Medical marijuana is being used clinically to manage pain because anti-inflammatory drugs and opioids are not always effective and come with side effects like dependence.3 Despite their increased use, the mechanism of how cannabinoids reduce pain is not well known. Therefore, the MMACRC is performing preclinical studies with rodents to determine how cannabinoids can effectively reduce pain in different models, including chemotherapy-induced pain. In their research, THC, CBD, and CBG compounds all decrease sensitivity to pain after chemotherapy. 4,5 This research is clinically relevant because chronic treatment with chemotherapy drugs can damage the nervous system and cause pain as a lasting side effect. CBD and CBG have also been shown to reduce pain from bone fractures comparable to traditional pain medications.6 By understanding the mechanisms of how cannabinoids decrease pain, researchers can develop better medications to manage pain. And if cannabinoids can reduce pain, then medical marijuana could potentially be used as an alternative to the current prescription of medications like opioids.
In addition to pain management, cannabinoids may be used as a treatment for different conditions. For example, cannabinoids have been explored as a treatment for cancer, as suggested by reduced cell viability in cancer cell lines, including colorectal cancer.7 In the studies on bone fracture, CBD and CBG were shown to promote bone healing in addition to reducing pain after tibial fracture in mice.6 This enhanced healing may be due to decreased inflammation and improved motor control. These same beneficial effects were observed after treatment with CBD and CBG extracts in a mouse model of arthritis.8 The potential for cannabinoids to both treat disease and manage pain as a side effect could make cannabinoids a more favorable treatment option than traditional medications.
While these results are exciting, equally important are findings that highlight the potential risks of medical marijuana use. In healthy mice, the cannabinoid CBG significantly reduced blood pressure This drastic drop in blood pressure, which may cause dizziness, confusion, blurry vision, and fainting, could be an adverse side effect, highlights the importance of research into the potential dangers of using medical marijuana.9
Another instance where medical marijuana may be harmful is in interaction with other drugs. Dr. Paul Kocis, with the MMACRC, developed the website CANN-DIR (The Cannabinoid Drug Interaction Review) to “screen for potential drug-drug interactions” between cannabinoids and prescription medications with the goal of increasing safe medication use.10 This tool can be helpful in exploring interactions with FDA approved medication and cannabinoids for adult nonprescription use (Figure 3). The user-friendly website is available in 10 languages and has been accessed in 80 countries. Both healthcare providers and the public can use CANN-DIR to find information about cannabinoid interactions with over 225 commonly prescribed medications. CANN-DIR may also help to reduce the stigma associated with marijuana use and improve safety by increasing communication about marijuana between provider and patient.

Research on medical marijuana in humans is more difficult to conduct since marijuana is currently classified as a Schedule I controlled substance – the same class as heroin and ecstasy. The DEA defines such substances as having “no accepted medical use and high potential for abuse.” However, this regulation may soon be lessened. On August 30th, 2023 the US Department of Health and Human Services recommended that marijuana be reclassified as a Schedule III drug, recognizing its low abuse potential and wide variety of promising medical uses. Under the current law, clinical research on medical marijuana is mainly limited to retrospective studies in collaboration with clinicians, and prospective surveys which aim to track individuals over time. Despite these regulations, the MMACRC can facilitate successful clinical research on cannabinoids due to the collaborative nature of the center. In a retrospective study which surveyed hundreds of inflammatory bowel disease (IBD) patients, researchers identified a need to better understand how cannabis may affect IBD symptoms. 11 Ongoing prospective studies also shed light on public interest in medical marijuana research and the need for a better understanding of when medical marijuana is safe and when it may be harmful.
Goals
I ended our conversation by asking Dr. Vrana where he sees the Penn State MMACRC in the next five years. Dr. Vrana’s hope is to continue making a difference in the public through education and outreach. While it is important to do the research to better understand medical marijuana, it may be even more important for that information to reach the lay public by publications, presentations, and other forms. Research from the MMACRC has received recognition at international meetings and has interest from federal agencies. Dr. Vrana has also been featured by Katie Couric Media, founded by award-winning journalist Katie Couric, and written for The Conversation. These media outlets reach thousands of people every day and can be utilized to highlight the importance of cannabinoid safety.
Many questions still remain, including the mechanism of cannabinoid action for pain relief and treatment of disease, safety of cannabinoid compounds, how legalization of recreational marijuana may change the research landscape, and the effects of cannabis on children and adolescents. But the MMACRC has created an ecosystem in which researchers and the public can better address these unknowns. The MMACRC will continue to make a difference in the context of cannabinoid research, and hopefully, scientists, politicians, and the community can keep working together to make medical marijuana as safe as possible.
TL:DR
- Medical Marijuana Academic Clinical Research Centers (MMACRC) were created to study the benefits and drawbacks to medical marijuana use.
- The MMACRC at Penn State includes several departments and supports basic science and clinical research.
- The goal is to make medical marijuana research more accessible to scientists despite regulatory challenges, and to share information with the public.
References
- Legare, C. A., Raup-Konsavage, W. M., & Vrana, K. E. (2022). Therapeutic Potential of Cannabis, Cannabidiol, and Cannabinoid-Based Pharmaceuticals. Pharmacology, 107(3-4), 131–149. https://doi.org/10.1159/000521683
- Nachnani, R., Raup-Konsavage, W. M., & Vrana, K. E. (2021). The Pharmacological Case for Cannabigerol. The Journal of pharmacology and experimental therapeutics, 376(2), 204–212. https://doi.org/10.1124/jpet.120.000340
- Krebs, E. E., Gravely, A., Nugent, S., Jensen, A. C., DeRonne, B., Goldsmith, E. S., Kroenke, K., Bair, M. J., & Noorbaloochi, S. (2018). Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain: The SPACE Randomized Clinical Trial. JAMA, 319(9), 872–882. https://doi.org/10.1001/jama.2018.0899
- Sepulveda, D. E., Vrana, K. E., Graziane, N. M., & Raup-Konsavage, W. M. (2022). Combinations of Cannabidiol and Δ9-Tetrahydrocannabinol in Reducing Chemotherapeutic Induced Neuropathic Pain. Biomedicines, 10(10), 2548. https://doi.org/10.3390/biomedicines10102548
- Sepulveda, D. E., Morris, D. P., Raup-Konsavage, W. M., Sun, D., Vrana, K. E., & Graziane, N. M. (2022). Cannabigerol (CBG) attenuates mechanical hypersensitivity elicited by chemotherapy-induced peripheral neuropathy. European journal of pain (London, England), 26(9), 1950–1966. https://doi.org/10.1002/ejp.2016
- Khajuria, D. K., Karuppagounder, V., Nowak, I., Sepulveda, D. E., Lewis, G. S., C, C. N., Raup-Konsavage, W. M., Vrana, K. E., Kamal, F., & Elbarbary, R. A. (2023). Cannabidiol and cannabigerol, non-psychotropic cannabinoids, as analgesics that effectively manage bone fracture pain and promote healing in mice. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research, 10.1002/jbmr.4902. Advance online publication. https://doi.org/10.1002/jbmr.4902
- Raup-Konsavage, W. M., Johnson, M., Legare, C. A., Yochum, G. S., Morgan, D. J., & Vrana, K. E. (2018). Synthetic Cannabinoid Activity Against Colorectal Cancer Cells. Cannabis and cannabinoid research, 3(1), 272–281. https://doi.org/10.1089/can.2018.0065
- Karuppagounder, V., Chung, J., Abdeen, A., Thompson, A., Bouboukas, A., Pinamont, W. J., Yoshioka, N. K., Sepulveda, D. E., Raup-Konsavage, W. M., Graziane, N. M., Vrana, K. E., Elbarbary, R. A., & Kamal, F. (2022). Distinctive Therapeutic Effects of Non-Euphorigenic Cannabis Extracts in Osteoarthritis. Cannabis and cannabinoid research, 10.1089/can.2021.0244. Advance online publication. https://doi.org/10.1089/can.2021.0244
- Vernail, V. L., Bingaman, S. S., Silberman, Y., Raup-Konsavage, W. M., Vrana, K. E., & Arnold, A. C. (2022). Acute Cannabigerol Administration Lowers Blood Pressure in Mice. Frontiers in physiology, 13, 871962. https://doi.org/10.3389/fphys.2022.871962
- Kocis, P. T., Wadrose, S., Wakefield, R. L., Ahmed, A., Calle, R., Gajjar, R., & Vrana, K. E. (2023). CANNabinoid Drug Interaction Review (CANN-DIR™). Medical cannabis and cannabinoids, 6(1), 1–7. https://doi.org/10.1159/000528528
- Coates, M. D., Dalessio, S., Walter, V., Stuart, A., Bernasko, N., Tinsley, A., Razeghi, S., Williams, E. D., Clarke, K., & Vrana, K. (2022). Symptoms and Extraintestinal Manifestations in Active Cannabis Users with Inflammatory Bowel Disease. Cannabis and cannabinoid research, 7(4), 445–450. https://doi.org/10.1089/can.2020.0155